DESCARGAR
VERSIÓN EXTENSA
DESCARGAR
VERSIÓN CORTA
DESCARGAR
RECOMENDACIONES Y FLUJOGRAMAS
vacio
vacio
Ámbito
- Esta guía debe ser usada en todos los establecimientos del seguro social del Perú (EsSalud), según lo correspondiente a su nivel de atención.
Población y alcance
- Población: pacientes en quienes se planea un procedimiento quirúrgico.
- Alcance: profilaxis antibiótica en procedimientos quirúrgicos.
Autores
Expertos clínicos:
-
Julio César Chamán Castillo
Hospital Edgardo Rebagliati Martins, EsSalud -
Hally Pacheco Oviedo
Red Asistencial Apurímac, EsSalud -
Henry Paucar Olivera
Red Asistencial Madre de Dios, EsSalud -
Fernando Villegas Paredes
Red Asistencial Arequipa, EsSalud -
Ysabel Chavez Santillán
Hospital Nacional Alberto Sabogal Sologuren, EsSalud -
Susana Aranzabal Durand
Hospital Nacional Edgardo Rebagliati Martins, EsSalud -
Martín Oyanguren Miranda
Hospital Nacional Edgardo Rebagliati Martins, EsSalud -
Ricardo Miguel Carpio Guzmán
Hospital Nacional Edgardo Rebagliati Martins, EsSalud -
Hugo Pedro Llerena Miranda
Hospital Nacional Edgardo Rebagliati Martins, EsSalud
Metodólogos:
-
César Ugarte Gil
Consultor Metodológico IETSI, EsSalud -
Maria Lazo Porras
Consultor Metodológico IETSI, EsSalud
Coordinadores:
-
Víctor Suárez Moreno
IETSI, EsSalud -
Raúl Timaná Ruiz
IETSI, EsSalud
Descargar PDF con más información sobre la filiación y rol de los autores.
Metodología
Resumen de la metodología:
- Conformación del GEG: La Dirección de Guías de Práctica Clínica, Farmacovigilancia y Tecnovigilancia, del Instituto de Evaluación de Tecnologías en Salud e Investigación (IETSI) del Seguro Social del Perú (EsSalud), conformó un grupo elaborador de la guía (GEG), que incluyó médicos especialistas y metodólogos.
- Planteamiento de preguntas clínicas: En concordancia con los objetivos y alcances de esta GPC, se formularon las preguntas clínicas.
- Búsqueda de la evidencia para cada pregunta: Para cada pregunta clínica, se realizaron búsquedas de revisiones sistemáticas (publicadas como artículos científicos o guías de práctica clínica). De no encontrar revisiones de calidad, se buscaron estudios primarios, cuyo riesgo de sesgo fue evaluado usando herramientas estandarizadas.
- Evaluación de la certeza de la evidencia: Para graduar la certeza de la evidencia, se siguió la metodología Grading of Recommendations Assessment, Development, and Evaluation (GRADE), y se usaron tablas de Summary of Findings (SoF).
- Formulación de las recomendaciones: El GEG revisó la evidencia recolectada para cada una de las preguntas clínicas en reuniones periódicas, en las que formuló las recomendaciones usando la metodología GRADE, otorgándole una fuerza a cada una. Para ello, se tuvo en consideración los beneficios y daños de las opciones, valores y preferencias de los pacientes, aceptabilidad, factibilidad, equidad y uso de recursos. Estos criterios fueron presentados y discutidos, tomando una decisión por consenso o mayoría simple. Asimismo, el GEG emitió puntos de buenas prácticas clínicas (BPC) sin una evaluación formal de la evidencia, y mayormente en base a su experiencia clínica.
- Revisión externa: La presente GPC fue revisada en reuniones con profesionales representantes de otras instituciones, tomadores de decisiones, y expertos externos.
Recomendaciones que resumen el contenido de la GPC
vacio
vacio
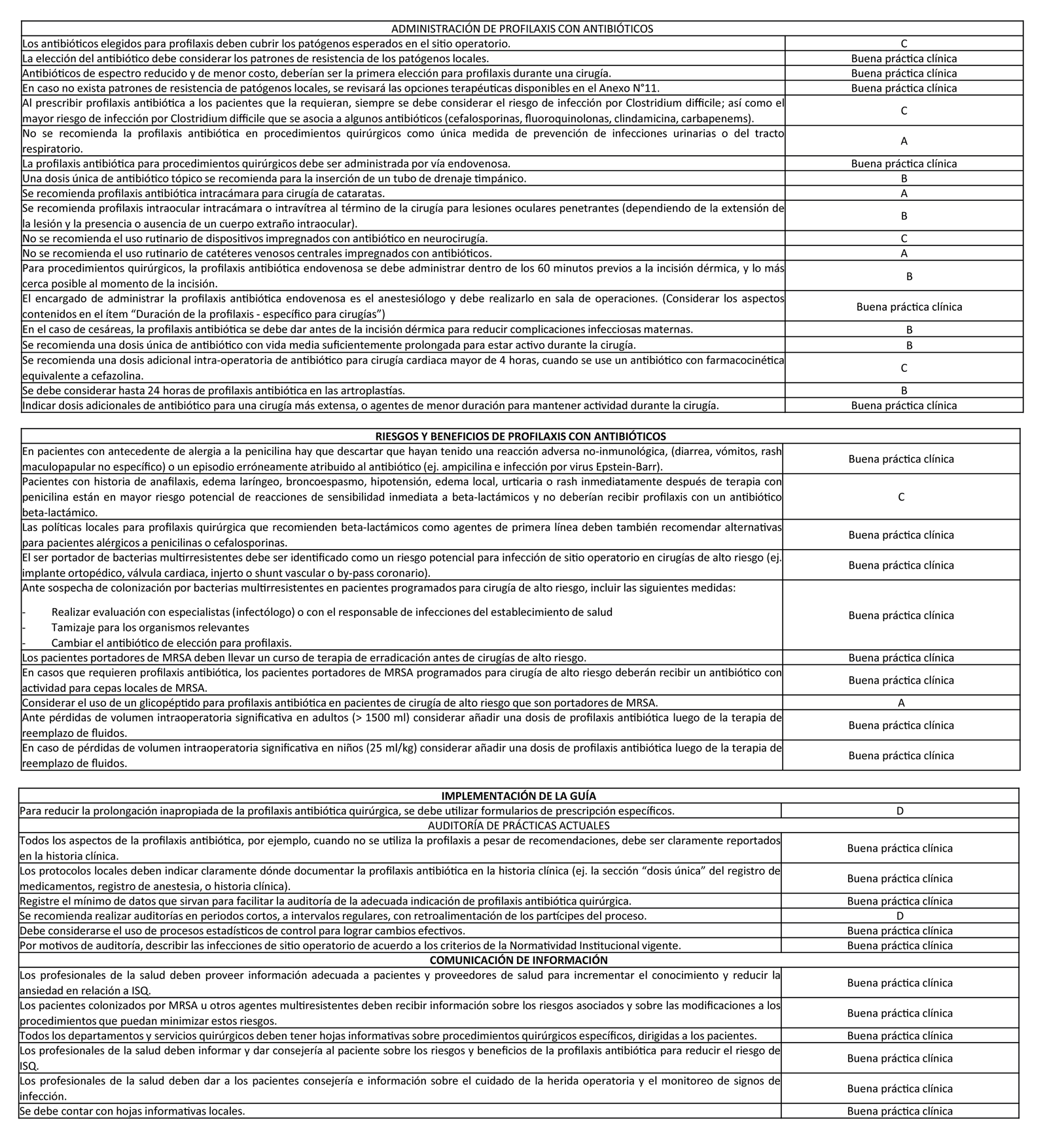
1. Principios generales de la profilaxis
Descargar PDF con el desarrollo de la pregunta.
Recomendación 1:
Una única dosis terapéutica estándar de antibiótico es suficiente para la profilaxis en la mayoría de circunstancias.
(Recomendación D)
BPC 1:
La decisión final en relación a los beneficios y riesgos de la profilaxis en un paciente individual dependerá de:
- el riesgo del paciente para la infección de sitio quirúrgico (ISQ)
- la potencial severidad de las consecuencias de ISQ
- la efectividad de la profilaxis para una cirugía específica
- las consecuencias de profilaxis en el paciente (por ejemplo, incremento de las infecciones por Clostridium difficile y otros organismos multirresistentes, así como reacciones adversas a medicamentos).
2. Administración de profilaxis con antibióticos
Descargar PDF con el desarrollo de la pregunta.
Recomendación 1:
Los antibióticos elegidos para profilaxis deben cubrir los patógenos esperados en el sitio operatorio.
(Recomendación C)
Recomendación 2:
Al prescribir profilaxis antibiótica a los pacientes que la requieran, siempre se debe considerar el riesgo de infección por Clostridium difficile; así como el mayor riesgo de infección por Clostridium difficile que se asocia a algunos antibióticos (cefalosporinas, fluoroquinolonas, clindamicina, carbapenems).
(Recomendación C)
Recomendación 3:
No se recomienda la profilaxis antibiótica en procedimientos quirúrgicos como única medida de prevención de infecciones urinarias o del tracto respiratorio.
(Recomendación A)
Recomendación 4:
Una dosis única de antibiótico tópico se recomienda para la inserción de un tubo de drenaje timpánico.
(Recomendación B)
Recomendación 5:
Se recomienda profilaxis antibiótica intracámara para cirugía de cataratas.
(Recomendación A)
Recomendación 6:
Se recomienda profilaxis intraocular intracámara o intravítrea al término de la cirugía para lesiones oculares penetrantes (dependiendo de la extensión de la lesión y la presencia o ausencia de un cuerpo extraño intraocular).
(Recomendación B)
Recomendación 7:
No se recomienda el uso rutinario de dispositivos impregnados con antibiótico en neurocirugía.
(Recomendación C)
Recomendación 8:
No se recomienda el uso rutinario de catéteres venosos centrales impregnados con antibióticos.
(Recomendación A)
Recomendación 9:
Para procedimientos quirúrgicos, la profilaxis antibiótica endovenosa se debe administrar dentro de los 60 minutos previos a la incisión dérmica, y lo más cerca posible al momento de la incisión.
(Recomendación B)
Recomendación 10:
En el caso de cesáreas, la profilaxis antibiótica se debe dar antes de la incisión dérmica para reducir complicaciones infecciosas maternas. (Recomendación B)
Recomendación 11:
Se recomienda una dosis única de antibiótico con vida media suficientemente prolongada para estar activo durante la cirugía.
(Recomendación B)
Recomendación 12:
Se recomienda una dosis adicional intra-operatoria de antibiótico para cirugía cardiaca mayor de 4 horas, cuando se use un antibiótico con farmacocinética equivalente a cefazolina.
(Recomendación C)
Recomendación 13:
Se debe considerar hasta 24 horas de profilaxis antibiótica en las artroplastías.
(Recomendación B)
BPC 1:
La elección del antibiótico debe considerar los patrones de resistencia de los patógenos locales.
BPC 2:
Antibióticos de espectro reducido y de menor costo, deberían ser la primera elección para profilaxis durante una cirugía.
BPC 3:
En caso no exista patrones de resistencia de patógenos locales, se revisará las opciones terapéuticas disponibles en el Anexo N°11.
BPC 4:
La profilaxis antibiótica para procedimientos quirúrgicos debe ser administrada por vía endovenosa.
BPC 5:
El encargado de administrar la profilaxis antibiótica endovenosa es el anestesiólogo y debe realizarlo en sala de operaciones. (Considerar los aspectos contenidos en el ítem “Duración de la profilaxis – específico para cirugías”)
BPC 6:
Indicar dosis adicionales de antibiótico para una cirugía más extensa, o agentes de menor duración para mantener actividad durante la cirugía.
3. Riesgos y beneficios de profilaxis con antibióticos
Descargar PDF con el desarrollo de la pregunta.
Recomendación 1:
Pacientes con historia de anafilaxis, edema laríngeo, broncoespasmo, hipotensión, edema local, urticaria o rash inmediatamente después de terapia con penicilina están en mayor riesgo potencial de reacciones de sensibilidad inmediata a beta-lactámicos y no deberían recibir profilaxis con un antibiótico beta-lactámico.
(Recomendación C)
Recomendación 2:
Considerar el uso de un glicopéptido para profilaxis antibiótica en pacientes de cirugía de alto riesgo que son portadores de MRSA.
(Recomendación A)
BPC 1:
En pacientes con antecedente de alergia a la penicilina hay que descartar que hayan tenido una reacción adversa no-inmunológica, (diarrea, vómitos, rash maculopapular no específico) o un episodio erróneamente atribuido al antibiótico (ej. ampicilina e infección por virus Epstein-Barr).
BPC 2:
Las políticas locales para profilaxis quirúrgica que recomienden beta-lactámicos como agentes de primera línea deben también recomendar alternativas para pacientes alérgicos a penicilinas o cefalosporinas.
BPC 3:
El ser portador de bacterias multirresistentes debe ser identificado como un riesgo potencial para infección de sitio operatorio en cirugías de alto riesgo (ej. implante ortopédico, válvula cardiaca, injerto o shunt vascular o by-pass coronario).
BPC 4:
Ante sospecha de colonización por bacterias multirresistentes en pacientes programados para cirugía de alto riesgo, incluir las siguientes medidas:
- Realizar evaluación con especialistas (infectólogo) o con el responsable de infecciones del establecimiento de salud
- Tamizaje para los organismos relevantes
- Cambiar el antibiótico de elección para profilaxis.
BPC 5:
Los pacientes portadores de MRSA deben llevar un curso de terapia de erradicación antes de cirugías de alto riesgo.
BPC 6:
En casos que requieren profilaxis antibiótica, los pacientes portadores de MRSA programados para cirugía de alto riesgo deberán recibir un antibiótico con actividad para cepas locales de MRSA.
BPC 7:
Ante pérdidas de volumen intraoperatoria significativa en adultos (> 1500 ml) considerar añadir una dosis de profilaxis antibiótica luego de la terapia de reemplazo de fluidos.
BPC 8:
En caso de pérdidas de volumen intraoperatoria significativa en niños (25 ml/kg) considerar añadir una dosis de profilaxis antibiótica luego de la terapia de reemplazo de fluidos.
4. Implementación de la guía
Descargar PDF con el desarrollo de la pregunta.
Recomendación 1:
Para reducir la prolongación inapropiada de la profilaxis antibiótica quirúrgica, se debe utilizar formularios de prescripción específicos.
(Recomendación D)
5. Auditoría de prácticas actuales
Descargar PDF con el desarrollo de la pregunta.
Recomendación 1:
Se recomienda realizar auditorías en periodos cortos, a intervalos regulares, con retroalimentación de los partícipes del proceso.
(Recomendación D)
BCP 1:
Todos los aspectos de la profilaxis antibiótica, por ejemplo, cuando no se utiliza la profilaxis a pesar de recomendaciones, debe ser claramente reportados en la historia clínica.
BCP 2:
Los protocolos locales deben indicar claramente dónde documentar la profilaxis antibiótica en la historia clínica (ej. la sección “dosis única” del registro de medicamentos, registro de anestesia, o historia clínica).
BPC 3:
Registre el mínimo de datos que sirvan para facilitar la auditoría de la adecuada indicación de profilaxis antibiótica quirúrgica.
BPC 4:
Debe considerarse el uso de procesos estadísticos de control para lograr cambios efectivos.
BPC 5:
Por motivos de auditoría, describir las infecciones de sitio operatorio de acuerdo a los criterios de la Normatividad Institucional vigente.
6. Comunicación de información
Descargar PDF con el desarrollo de la pregunta.
BPC 1:
Los profesionales de la salud deben proveer información adecuada a pacientes y proveedores de salud para incrementar el conocimiento y reducir la ansiedad en relación a ISQ.
BPC 2:
Los pacientes colonizados por MRSA u otros agentes multiresistentes deben recibir información sobre los riesgos asociados y sobre las modificaciones a los procedimientos que puedan minimizar estos riesgos.
BPC 3:
Todos los departamentos y servicios quirúrgicos deben tener hojas informativas sobre procedimientos quirúrgicos específicos, dirigidas a los pacientes.
BPC 4:
Los profesionales de la salud deben informar y dar consejería al paciente sobre los riesgos y beneficios de la profilaxis antibiótica para reducir el riesgo de ISQ.
BPC 5:
Los profesionales de la salud deben dar a los pacientes consejería e información sobre el cuidado de la herida operatoria y el monitoreo de signos de infección.
BPC 6:
Se debe contar con hojas informativas locales.
Referencias bibliográficas
- Leaper D, Ousey K. Evidence update on prevention of surgical site infection. Current opinion in infectious diseases. 2015;28(2):158-63.
- Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infection control and hospital epidemiology. 1992;13(10):606-8.
- Lewis SS, Moehring RW, Chen LF, Sexton DJ, Anderson DJ. Assessing the relative burden of hospital-acquired infections in a network of community hospitals. Infection control and hospital epidemiology. 2013;34(11):1229-30.
- Najjar PA, Smink DS. Prophylactic antibiotics and prevention of surgical site infections. The Surgical clinics of North America. 2015;95(2):269-83.
- Hidalgo LF, Marroquín JE, Antigoni J, Samalvides F. Prevalencia de infecciones hospitalarias en un hospital peruano de nivel IV, en el año 2008. Revista Medica Herediana. 2011;22(2):76-81.
- Murga Valdéz MA. Infección de sitio operatorio en pacientes obesas y no obesas sometidas a Histerectomía vaginal en el servicio de ginecología del Hospital Nacional Arzobispo Loayza. 2009.
- Avalos Chicata JM. National Nosocomial Infections Surveillance (NNIS) como Índice de riesgo en la predicción de infección del sitio quirúrgico en pacientes apendicectomizados. Hospital Regional Docente de Trujillo. 2013.
- MINSA. GUIAS DE PRÁCTICA CLINICA – SERVICIO DE CIRUGIA GENERAL. Hospital Santa Rosa; 2009.
- MINSA. GUIAS DE PRÁCTICA CLINICA – SERVICIO DE CIRUGIA GENERAL. Hospital de Emergencias Jose Casimiro Ulloa; 2011.
- MINSA. GUIAS DE PRÁCTICA CLINICA – SERVICIO DE CIRUGIA GENERAL. Hospital Santa Rosa; 2015.
- Directiva para el Desarrollo de las Guías de Práctica Clínica en ESSALUD, (2016).
- Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. American journal of health-system pharmacy : AJHP : official journal of the American Society of Health-System Pharmacists. 2013;70(3):195-283.
- SIGN. SIGN 104 • Antibiotic prophylaxis in surgery. Edinburgh: Scottish Intercollegiate Guidelines Network; 2014.
- National Guideline C. Surgical site infection: prevention and treatment of surgical site infection. 2008.
- Health NIf, Excellence C. Surgical site infection: prevention and treatment of surgical site infection: National Institute for Health and Clinical Excellence; 2008.
- Khashab MA, Chithadi KV, Acosta RD, Bruining DH, Chandrasekhara V, Eloubeidi MA, et al. Antibiotic prophylaxis for GI endoscopy. Gastrointestinal endoscopy. 2015;81(1):81-9.
- Shaffer WO, Baisden JL, Fernand R, Matz PG. An evidence-based clinical guideline for antibiotic prophylaxis in spine surgery. The spine journal : official journal of the North American Spine Society. 2013;13(10):1387-92.
- MINSA. Documento Técnico: «Metodología para la elaboración de Guías de Práctica Clínica». Lima, Perú: Ministerio de Salud. Dirección General de Salud de las Personas; 2015. p. 1-53.
- Harbour R, Miller J. A new system for grading recommendations in evidence based guidelines. BMJ (Clinical research ed). 2001;323(7308):334-6.
- SIGN. SIGN 50 • A guideline developer’s handbook Edinburgh: Scottish Intercollegiate Guidelines Network; 2011.
- Baum ML, Anish DS, Chalmers TC, Sacks HS, Smith H, Jr., Fagerstrom RM. A survey of clinical trials of antibiotic prophylaxis in colon surgery: evidence against further use of no-treatment controls. The New England journal of medicine. 1981;305(14):795-9.
- Lidwell OM. Air, antibiotics and sepsis in replacement joints. The Journal of hospital infection. 1988;11 Suppl C:18-40.
- Davey PG, Duncan ID, Edward D, Scott AC. Cost-benefit analysis of cephradine and mezlocillin prophylaxis for abdominal and vaginal hysterectomy. British journal of obstetrics and gynaecology. 1988;95(11):1170-7.
- Avery CM, Ameerally P, Castling B, Swann RA. Infection of surgical wounds in the maxillofacial region and free flap donor sites with methicillin-resistant Staphylococcus aureus. The British journal of oral & maxillofacial surgery. 2006;44(3):217-21.
- Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for Prevention of Surgical Site Infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. American journal of infection control. 1999;27(2):97-132; quiz 3-4; discussion 96.
- Dietrich ES, Bieser U, Frank U, Schwarzer G, Daschner FD. Ceftriaxone versus other cephalosporins for perioperative antibiotic prophylaxis: a meta-analysis of 43 randomized controlled trials. Chemotherapy. 2002;48(1):49-56.
- Esposito S, Noviello S, Vanasia A, Venturino P. Ceftriaxone versus Other Antibiotics for Surgical Prophylaxis : A Meta-Analysis. Clinical drug investigation. 2004;24(1):29-39.
- Bolon MK, Morlote M, Weber SG, Koplan B, Carmeli Y, Wright SB. Glycopeptides are no more effective than beta-lactam agents for prevention of surgical site infection after cardiac surgery: a meta-analysis. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2004;38(10):1357-63.
- Nelson RL, Kelsey P, Leeman H, Meardon N, Patel H, Paul K, et al. Antibiotic treatment for Clostridium difficile-associated diarrhea in adults. The Cochrane database of systematic reviews. 2011(9):Cd004610.
- Howell MD, Novack V, Grgurich P, Soulliard D, Novack L, Pencina M, et al. Iatrogenic gastric acid suppression and the risk of nosocomial Clostridium difficile infection. Archives of internal medicine. 2010;170(9):784-90.
- Poutanen SM, Simor AE. Clostridium difficile-associated diarrhea in adults. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne. 2004;171(1):51-8.
- Southern WN, Rahmani R, Aroniadis O, Khorshidi I, Thanjan A, Ibrahim C, et al. Postoperative Clostridium difficile-associated diarrhea. Surgery. 2010;148(1):24-30.
- Vernaz N, Hill K, Leggeat S, Nathwani D, Philips G, Bonnabry P, et al. Temporal effects of antibiotic use and Clostridium difficile infections. The Journal of antimicrobial chemotherapy. 2009;63(6):1272-5.
- Zipfel TE, Wood WE, Street DF, Wulffman J, Tipirneni A, Frey C, et al. The effect of topical ciprofloxacin on postoperative otorrhea after tympanostomy tube insertion. The American journal of otology. 1999;20(4):416-20.
- Nawasreh O, Al-Wedyan IA. Prophylactic ciprofloxacin drops after tympanostomy tube insertion. Saudi medical journal. 2004;25(1):38-40.
- Seal DV, Barry P, Gettinby G, Lees F, Peterson M, Revie CW, et al. ESCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery: Case for a European multicenter study. Journal of cataract and refractive surgery. 2006;32(3):396-406.
- Narang S, Gupta V, Gupta A, Dogra MR, Pandav SS, Das S. Role of prophylactic intravitreal antibiotics in open globe injuries. Indian journal of ophthalmology. 2003;51(1):39-44.
- Soheilian M, Rafati N, Mohebbi MR, Yazdani S, Habibabadi HF, Feghhi M, et al. Prophylaxis of acute posttraumatic bacterial endophthalmitis: a multicenter, randomized clinical trial of intraocular antibiotic injection, report 2. Archives of ophthalmology (Chicago, Ill : 1960). 2007;125(4):460-5.
- Zabramski JM, Whiting D, Darouiche RO, Horner TG, Olson J, Robertson C, et al. Efficacy of antimicrobial-impregnated external ventricular drain catheters: a prospective, randomized, controlled trial. Journal of neurosurgery. 2003;98(4):725-30.
- Sciubba DM, Stuart RM, McGirt MJ, Woodworth GF, Samdani A, Carson B, et al. Effect of antibiotic-impregnated shunt catheters in decreasing the incidence of shunt infection in the treatment of hydrocephalus. Journal of neurosurgery. 2005;103(2 Suppl):131-6.
- Govender ST, Nathoo N, van Dellen JR. Evaluation of an antibiotic-impregnated shunt system for the treatment of hydrocephalus. Journal of neurosurgery. 2003;99(5):831-9.
- Aryan HE, Meltzer HS, Park MS, Bennett RL, Jandial R, Levy ML. Initial experience with antibiotic-impregnated silicone catheters for shunting of cerebrospinal fluid in children. Child’s nervous system : ChNS : official journal of the International Society for Pediatric Neurosurgery. 2005;21(1):56-61.
- Marin MG, Lee JC, Skurnick JH. Prevention of nosocomial bloodstream infections: effectiveness of antimicrobial-impregnated and heparin-bonded central venous catheters. Crit Care Med. 2000;28(9):3332-8.
- Raad I, Darouiche R, Dupuis J, Abi-Said D, Gabrielli A, Hachem R, et al. Central venous catheters coated with minocycline and rifampin for the prevention of catheter-related colonization and bloodstream infections. A randomized, double-blind trial. The Texas Medical Center Catheter Study Group. Annals of internal medicine. 1997;127(4):267-74.
- Milstone AM, Maragakis LL, Townsend T, Speck K, Sponseller P, Song X, et al. Timing of preoperative antibiotic prophylaxis: a modifiable risk factor for deep surgical site infections after pediatric spinal fusion. The Pediatric infectious disease journal. 2008;27(8):704-8.
- Koch CG, Li L, Hixson E, Tang A, Gordon S, Longworth D, et al. Is it time to refine? An exploration and simulation of optimal antibiotic timing in general surgery. Journal of the American College of Surgeons. 2013;217(4):628-35.
- Organization WH. Global guidelines for the prevention of surgical site infection: World Health Organization; 2016.
- Berríos-Torres SI, Umscheid CA, Bratzler DW, et al. Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surgery. 2017;152(8):784-91.
- Tita AT, Rouse DJ, Blackwell S, Saade GR, Spong CY, Andrews WW. Emerging concepts in antibiotic prophylaxis for cesarean delivery: a systematic review. Obstetrics and gynecology. 2009;113(3):675-82.
- Kaimal AJ, Zlatnik MG, Cheng YW, Thiet MP, Connatty E, Creedy P, et al. Effect of a change in policy regarding the timing of prophylactic antibiotics on the rate of postcesarean delivery surgical-site infections. American journal of obstetrics and gynecology. 2008;199(3):310.e1-5.
- Mui LM, Ng CS, Wong SK, Lam YH, Fung TM, Fok KL, et al. Optimum duration of prophylactic antibiotics in acute non-perforated appendicitis. ANZ journal of surgery. 2005;75(6):425-8.
- Velmahos GC, Toutouzas KG, Sarkisyan G, Chan LS, Jindal A, Karaiskakis M, et al. Severe trauma is not an excuse for prolonged antibiotic prophylaxis. Archives of surgery (Chicago, Ill : 1960). 2002;137(5):537-41; discussion 41-2.
- Song F, Glenny AM. Antimicrobial prophylaxis in colorectal surgery: a systematic review of randomised controlled trials. Health technology assessment (Winchester, England). 1998;2(7):1-110.
- Zanetti G, Giardina R, Platt R. Intraoperative redosing of cefazolin and risk for surgical site infection in cardiac surgery. Emerging infectious diseases. 2001;7(5):828-31.
- Engesaeter LB, Lie SA, Espehaug B, Furnes O, Vollset SE, Havelin LI. Antibiotic prophylaxis in total hip arthroplasty: effects of antibiotic prophylaxis systemically and in bone cement on the revision rate of 22,170 primary hip replacements followed 0-14 years in the Norwegian Arthroplasty Register. Acta orthopaedica Scandinavica. 2003;74(6):644-51.
- Sogn DD. Penicillin allergy. The Journal of allergy and clinical immunology. 1984;74(4 Pt 2):589-93.
- Saxon A, Adelman DC, Patel A, Hajdu R, Calandra GB. Imipenem cross-reactivity with penicillin in humans. The Journal of allergy and clinical immunology. 1988;82(2):213-7.
- Dehne MG, Muhling J, Sablotzki A, Nopens H, Hempelmann G. Pharmacokinetics of antibiotic prophylaxis in major orthopedic surgery and blood-saving techniques. Orthopedics. 2001;24(7):665-9.
- Wollinsky KH, Buchele M, Oethinger M, Kluger P, Mehrkens HH, Marre R, et al. Influence of hemodilution on cefuroxime levels and bacterial contamination of intra- and postoperative processed wound blood during hip replacement. Beitrage zur Infusionstherapie und Transfusionsmedizin = Contributions to infusion therapy and transfusion medicine. 1996;33:191-5.
- Levy M, Egersegi P, Strong A, Tessoro A, Spino M, Bannatyne R, et al. Pharmacokinetic analysis of cloxacillin loss in children undergoing major surgery with massive bleeding. Antimicrobial agents and chemotherapy. 1990;34(6):1150-3.
- Swoboda SM, Merz C, Kostuik J, Trentler B, Lipsett PA. Does intraoperative blood loss affect antibiotic serum and tissue concentrations? Archives of surgery (Chicago, Ill : 1960). 1996;131(11):1165-71; discussion 71-2.
- WHO, UNICEF. Managing complications in pregnancy and childbirth: a guide for midwives and doctors. 2007.
- Davey P, Napier A, McMillan J, Ruta D. Audit of antibiotic prophylaxis for surgical patients in three hospital trusts in Tayside. Tayside Area Clinical Audit Commitee. Health bulletin. 1999;57(2):118-27.
- Alerany C, Campany D, Monterde J, Semeraro C. Impact of local guidelines and an integrated dispensing system on antibiotic prophylaxis quality in a surgical centre. The Journal of hospital infection. 2005;60(2):111-7.
- Carles M, Gindre S, Aknouch N, Goubaux B, Mousnier A, Raucoules-Aime M. Improvement of surgical antibiotic prophylaxis: a prospective evaluation of personalized antibiotic kits. The Journal of hospital infection. 2006;62(3):372-5.
- Pons-Busom M, Aguas-Compaired M, Delas J, Eguileor-Partearroyo B. Compliance with local guidelines for antibiotic prophylaxis in surgery. Infection control and hospital epidemiology. 2004;25(4):308-12.
- Thor J, Lundberg J, Ask J, Olsson J, Carli C, Harenstam KP, et al. Application of statistical process control in healthcare improvement: systematic review. Quality & safety in health care. 2007;16(5):387-99.
- Bruce J, Russell EM, Mollison J, Krukowski ZH. The measurement and monitoring of surgical adverse events. Health technology assessment (Winchester, England). 2001;5(22):1-194.
- Barker FG, 2nd. Efficacy of prophylactic antibiotics for craniotomy: a meta-analysis. 1994(0148-396X (Print)).
- Haines SJ, Walters BC. Antibiotic prophylaxis for cerebrospinal fluid shunts: a metanalysis. 1994(0148-396X (Print)).
- Langley JM, LeBlanc Jc Fau – Drake J, Drake J Fau – Milner R, Milner R. Efficacy of antimicrobial prophylaxis in placement of cerebrospinal fluid shunts: meta-analysis. 1993(1058-4838 (Print)).
- Barker FG, 2nd. Efficacy of prophylactic antibiotic therapy in spinal surgery: a meta-analysis. 2002(0148-396X (Print)).
- Prophylaxis of postoperative endophthalmitis following cataract surgery: results of the ESCRS multicenter study and identification of risk factors. Journal of cataract and refractive surgery. 2007;33(6):978-88.
- Vardy SJ, Rose GE. Prevention of cellulitis after open lacrimal surgery: a prospective study of three methods. Ophthalmology. 2000;107(2):315-7.
- Andreasen JO, Jensen SS, Schwartz O, Hillerup Y. A systematic review of prophylactic antibiotics in the surgical treatment of maxillofacial fractures. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 2006;64(11):1664-8.
- Zallen RD, Curry JT. A study of antibiotic usage in compound mandibular fractures. Journal of oral surgery (American Dental Association : 1965). 1975;33(6):431-4.
- Lindeboom JA, Frenken JW, Tuk JG, Kroon FH. A randomized prospective controlled trial of antibiotic prophylaxis in intraoral bone-grafting procedures: preoperative single-dose penicillin versus preoperative single-dose clindamycin. International journal of oral and maxillofacial surgery. 2006;35(5):433-6.
- Baqain ZH, Hyde N, Patrikidou A, Harris M. Antibiotic prophylaxis for orthognathic surgery: a prospective, randomised clinical trial. The British journal of oral & maxillofacial surgery. 2004;42(6):506-10.
- Bentley KC, Head TW, Aiello GA. Antibiotic prophylaxis in orthognathic surgery: a 1-day versus 5-day regimen. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 1999;57(3):226-30; discussion 30-2.
- Fridrich KL, Partnoy BE, Zeitler DL. Prospective analysis of antibiotic prophylaxis for orthognathic surgery. The International journal of adult orthodontics and orthognathic surgery. 1994;9(2):129-31.
- Zijderveld SA, Smeele LE, Kostense PJ, Tuinzing DB. Preoperative antibiotic prophylaxis in orthognathic surgery: a randomized, double-blind, and placebo-controlled clinical study. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons. 1999;57(12):1403-6; discussion 6-7.
- Dellinger EP, Gross PA, Barrett TL, Krause PJ, Martone WJ, McGowan JE, Jr., et al. Quality standard for antimicrobial prophylaxis in surgical procedures. Infectious Diseases Society of America. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 1994;18(3):422-7.
- Verschuur HP, de Wever WW, van Benthem PP. Antibiotic prophylaxis in clean and clean-contaminated ear surgery. The Cochrane database of systematic reviews. 2004(3):Cd003996.
- Annys E, Jorissen M. Short term effects of antibiotics (Zinnat) after endoscopic sinus surgery. Acta oto-rhino-laryngologica Belgica. 2000;54(1):23-8.
- Andrews PJ, East CA, Jayaraj SM, Badia L, Panagamuwa C, Harding L. Prophylactic vs postoperative antibiotic use in complex septorhinoplasty surgery: a prospective, randomized, single-blind trial comparing efficacy. Archives of facial plastic surgery. 2006;8(2):84-7.
- Sanchez-Carrion S, Prim MP, De Diego JI, Sastre N, Pena-Garcia P. Utility of prophylactic antibiotics in pediatric adenoidectomy. International journal of pediatric otorhinolaryngology. 2006;70(7):1275-81.
- Kocaturk S, Yardimci S, Yildirim A, Incesulu A. Preventive therapy for postoperative purulent otorrhea after ventilation tube insertion. American journal of otolaryngology. 2005;26(2):123-7.
- Johnson JT, Wagner RL. Infection following uncontaminated head and neck surgery. Archives of otolaryngology–head & neck surgery. 1987;113(4):368-9.
- Simo R, French G. The use of prophylactic antibiotics in head and neck oncological surgery. Current opinion in otolaryngology & head and neck surgery. 2006;14(2):55-61.
- Coskun H, Erisen L, Basut O. Factors affecting wound infection rates in head and neck surgery. Otolaryngology–head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck Surgery. 2000;123(3):328-33.
- Seven H, Sayin I, Turgut S. Antibiotic prophylaxis in clean neck dissections. The Journal of laryngology and otology. 2004;118(3):213-6.
- Becker GD, Parell GJ. Cefazolin prophylaxis in head and neck cancer surgery. The Annals of otology, rhinology, and laryngology. 1979;88(2 Pt 1):183-6.
- Dor P, Klastersky J. Prophylactic antibiotics in oral, pharyngeal and laryngeal surgery for cancer: (a double-blind study). The Laryngoscope. 1973;83(12):1992-8.
- Johnson JT, Yu VL, Myers EN, Muder RR, Thearle PB, Diven WF. Efficacy of two third-generation cephalosporins in prophylaxis for head and neck surgery. Archives of otolaryngology (Chicago, Ill : 1960). 1984;110(4):224-7.
- Velanovich V. A meta-analysis of prophylactic antibiotics in head and neck surgery. Plastic and reconstructive surgery. 1991;87(3):429-34; discussion 35.
- Cunningham M, Bunn F, Handscomb K. Prophylactic antibiotics to prevent surgical site infection after breast cancer surgery. The Cochrane database of systematic reviews. 2006(2):Cd005360.
- Ahmadi AH, Cohen BE, Shayani P. A prospective study of antibiotic efficacy in preventing infection in reduction mammaplasty. Plastic and reconstructive surgery. 2005;116(1):126-31.
- Da Costa A, Kirkorian G, Cucherat M, Delahaye F, Chevalier P, Cerisier A, et al. Antibiotic prophylaxis for permanent pacemaker implantation: a meta-analysis. Circulation. 1998;97(18):1796-801.
- Austin TW, Coles JC, Burnett R, Goldbach M. Aortocoronary bypass procedures and sternotomy infections: a study of antistaphylococcal prophylaxis. Canadian journal of surgery Journal canadien de chirurgie. 1980;23(5):483-5.
- Fong IW, Baker CB, McKee DC. The value of prophylactic antibiotics in aorat-coronary bypass operations: a double-blind randomized trial. The Journal of thoracic and cardiovascular surgery. 1979;78(6):908-13.
- Penketh AR, Wansbrough-Jones MH, Wright E, Imrie F, Pepper JR, Parker DJ. Antibiotic prophylaxis for coronary artery bypass graft surgery. Lancet (London, England). 1985;1(8444):1500.
- Harbarth S, Samore MH, Lichtenberg D, Carmeli Y. Prolonged antibiotic prophylaxis after cardiovascular surgery and its effect on surgical site infections and antimicrobial resistance. Circulation. 2000;101(25):2916-21.
- Aznar R, Mateu M, Miro JM, Gatell JM, Gimferrer JM, Aznar E, et al. Antibiotic prophylaxis in non-cardiac thoracic surgery: cefazolin versus placebo. European journal of cardio-thoracic surgery : official journal of the European Association for Cardio-thoracic Surgery. 1991;5(10):515-8.
- Ilves R, Cooper JD, Todd TR, Pearson FG. Prospective, randomized, double-blind study using prophylactic cephalothin for major, elective, general thoracic operations. The Journal of thoracic and cardiovascular surgery. 1981;81(6):813-7.
- Bricard H, Deshayes JP, Sillard B, Lefrancois C, Delassus P, Lochu T, et al. [Antibiotic prophylaxis in surgery of the esophagus]. Annales francaises d’anesthesie et de reanimation. 1994;13(5 Suppl):S161-8.
- Evans C, Pollock AV. The reduction of surgical wound infections by prophylactic parenteral cephaloridine. A controlled clinical trial. The British journal of surgery. 1973;60(6):434-7.
- Lewis RT, Allan CM, Goodall RG, Lloyd-Smith WC, Marien B, Wiegand FM. Discriminate use of antibiotic prophylaxis in gastroduodenal surgery. American journal of surgery. 1979;138(5):640-3.
- Polk HC, Jr., Lopez-Mayor JF. Postoperative wound infection: a prospective study of determinant factors and prevention. Surgery. 1969;66(1):97-103.
- Meijer WS, Schmitz PI, Jeekel J. Meta-analysis of randomized, controlled clinical trials of antibiotic prophylaxis in biliary tract surgery. The British journal of surgery. 1990;77(3):283-90.
- Catarci M, Mancini S, Gentileschi P, Camplone C, Sileri P, Grassi GB. Antibiotic prophylaxis in elective laparoscopic cholecystectomy. Lack of need or lack of evidence? Surgical endoscopy. 2004;18(4):638-41.
- Andersen BR, Kallehave FL, Andersen HK. Antibiotics versus placebo for prevention of postoperative infection after appendicectomy. The Cochrane database of systematic reviews. 2005(3):Cd001439.
- Aufenacker TJ, Koelemay MJ, Gouma DJ, Simons MP. Systematic review and meta-analysis of the effectiveness of antibiotic prophylaxis in prevention of wound infection after mesh repair of abdominal wall hernia. The British journal of surgery. 2006;93(1):5-10.
- Sanchez-Manuel FJ, Lozano-Garcia J, Seco-Gil JL. Antibiotic prophylaxis for hernia repair. The Cochrane database of systematic reviews. 2012(2):Cd003769.
- Antibiotic prophylaxis in gastrointestinal endoscopy London: British Society of Gastroenterology; 2001 [Available from: http://www.bsg.org.uk/pdf_word_docs/prophylaxis2001.pdf.
- Davies JM, Barnes R, Milligan D. Update of guidelines for the prevention and treatment of infection in patients with an absent or dysfunctional spleen. Clinical medicine (London, England). 2002;2(5):440-3.
- Mittendorf R, Aronson MP, Berry RE, Williams MA, Kupelnick B, Klickstein A, et al. Avoiding serious infections associated with abdominal hysterectomy: a meta-analysis of antibiotic prophylaxis. American journal of obstetrics and gynecology. 1993;169(5):1119-24.
- Tanos V, Rojansky N. Prophylactic antibiotics in abdominal hysterectomy. Journal of the American College of Surgeons. 1994;179(5):593-600.
- Allen JL, Rampone JF, Wheeless CR. Use of a prophylactic antibiotic in elective major gynecologic operations. Obstetrics and gynecology. 1972;39(2):218-24.
- Ledger WJ, Sweet RL, Headington JT. Prophylactic cephaloridine in the prevention of postoperative pelvic infections in premenopausal women undergoing vaginal hysterectomy. American journal of obstetrics and gynecology. 1973;115(6):766-74.
- Smaill F, Hofmeyr GJ. Antibiotic prophylaxis for cesarean section. The Cochrane database of systematic reviews. 2002(3):Cd000933.
- Liabsuetrakul T, Choobun T, Peeyananjarassri K, Islam QM. Antibiotic prophylaxis for operative vaginal delivery. The Cochrane database of systematic reviews. 2014(10):Cd004455.
- Adams E, Fernando R. Management of third-and fourth-degree perineal tears following vaginal delivery: Royal College of Obstetricians and Gynaecologists; 2001.
- Sawaya GF, Grady D, Kerlikowske K, Grimes DA. Antibiotics at the time of induced abortion: the case for universal prophylaxis based on a meta-analysis. Obstetrics and gynecology. 1996;87(5 Pt 2):884-90.
- May W, Gulmezoglu AM, Ba-Thike K. Antibiotics for incomplete abortion. The Cochrane database of systematic reviews. 2007(4):Cd001779.
- Grimes DA, Schulz KF. Prophylactic antibiotics for intrauterine device insertion: a metaanalysis of the randomized controlled trials. Contraception. 1999;60(2):57-63.
- Crawford ED, Haynes AL, Jr., Story MW, Borden TA. Prevention of urinary tract infection and sepsis following transrectal prostatic biopsy. The Journal of urology. 1982;127(3):449-51.
- Ruebush TK, 2nd, McConville JH, Calia FM. A double-blind study of trimethoprim-sulfamethoxazole prophylaxis in patients having transrectal needle biopsy of the prostate. The Journal of urology. 1979;122(4):492-4.
- Pearle MS, Roehrborn CG. Antimicrobial prophylaxis prior to shock wave lithotripsy in patients with sterile urine before treatment: a meta-analysis and cost-effectiveness analysis. Urology. 1997;49(5):679-86.
- Mariappan P, Smith G, Moussa SA, Tolley DA. One week of ciprofloxacin before percutaneous nephrolithotomy significantly reduces upper tract infection and urosepsis: a prospective controlled study. BJU international. 2006;98(5):1075-9.
- Knopf HJ, Graff HJ, Schulze H. Perioperative antibiotic prophylaxis in ureteroscopic stone removal. European urology. 2003;44(1):115-8.
- Takahashi S, Takeyama K, Miyamoto S, Tanuma Y, Takagi Y. Surgical antimicrobial prophylaxis in transurethral ureterolithotripsy. Journal of infection and chemotherapy : official journal of the Japan Society of Chemotherapy. 2005;11(5):239-43.
- Berry A, Barratt A. Prophylactic antibiotic use in transurethral prostatic resection: a meta-analysis. The Journal of urology. 2002;167(2 Pt 1):571-7.
- Delavierre D, Huiban B, Fournier G, Le Gall G, Tande D, Mangin P. [The value of antibiotic prophylaxis in transurethral resection of bladder tumors. Apropos of 61 cases]. Progres en urologie : journal de l’Association francaise d’urologie et de la Societe francaise d’urologie. 1993;3(4):577-82.
- Takeyama K, Matsukawa M, Kunishima Y, Takahashi S, Hotta H, Nishiyama N, et al. Incidence of and risk factors for surgical site infection in patients with radical cystectomy with urinary diversion. Journal of infection and chemotherapy : official journal of the Japan Society of Chemotherapy. 2005;11(4):177-81.
- Block JE, Stubbs HA. Reducing the risk of deep wound infection in primary joint arthroplasty with antibiotic bone cement. Orthopedics. 2005;28(11):1334-45.
- Hill C, Flamant R, Mazas F, Evrard J. Prophylactic cefazolin versus placebo in total hip replacement. Report of a multicentre double-blind randomised trial. Lancet (London, England). 1981;1(8224):795-6.
- Lidwell OM, Lowbury EJ, Whyte W, Blowers R, Stanley SJ, Lowe D. Effect of ultraclean air in operating rooms on deep sepsis in the joint after total hip or knee replacement: a randomised study. British medical journal (Clinical research ed). 1982;285(6334):10-4.
- Gosselin RA, Roberts I, Gillespie WJ. Antibiotics for preventing infection in open limb fractures. The Cochrane database of systematic reviews. 2004(1):Cd003764.
- Gillespie WJ, Walenkamp GH. Antibiotic prophylaxis for surgery for proximal femoral and other closed long bone fractures. The Cochrane database of systematic reviews. 2010(3):Cd000244.
- Southwell-Keely JP, Russo RR, March L, Cumming R, Cameron I, Brnabic AJ. Antibiotic prophylaxis in hip fracture surgery: a metaanalysis. Clinical orthopaedics and related research. 2004(419):179-84.
- Sonne-Holm S, Boeckstyns M, Menck H, Sinding A, Leicht P, Dichmann O, et al. Prophylactic antibiotics in amputation of the lower extremity for ischemia. A placebo-controlled, randomized trial of cefoxitin. The Journal of bone and joint surgery American volume. 1985;67(5):800-3.
- Stewart A, Eyers PS, Earnshaw JJ. Prevention of infection in arterial reconstruction. The Cochrane database of systematic reviews. 2006(3):Cd003073.
- O’Grady NP, Alexander M, Dellinger EP, Gerberding JL, Heard SO, Maki DG, et al. Guidelines for the prevention of intravascular catheter-related infections. Infection control and hospital epidemiology. 2002;23(12):759-69.
- Sharma VK, Howden CW. Meta-analysis of randomized, controlled trials of antibiotic prophylaxis before percutaneous endoscopic gastrostomy. The American journal of gastroenterology. 2000;95(11):3133-6.
- Meir DB, Livne PM. Is prophylactic antimicrobial treatment necessary after hypospadias repair? The Journal of urology. 2004;171(6 Pt 2):2621-2.
- van de Wetering MD, van Woensel JB, Kremer LC, Caron HN. Prophylactic antibiotics for preventing early Gram-positive central venous catheter infections in oncology patients, a Cochrane systematic review. Cancer treatment reviews. 2005;31(3):186-96.
- Conklin CM, Gray RJ, Neilson D, Wong P, Tomita DK, Matloff JM. Determinants of wound infection incidence after isolated coronary artery bypass surgery in patients randomized to receive prophylactic cefuroxime or cefazolin. Annals of Thoracic Surgery. 1988;46(2):172-7.
- Curtis JJ, Boley TM, Walls JT, Hamory B, Schmaltz RA. Randomized, prospective comparison of first- and second-generation cephalosporins as infection prophylaxis for cardiac surgery. The American Journal of Surgery. 1993;166(6):734-7.
- Doebbeling BN, Pfaller MA, Kuhns KR, Massanari RM, Behrendt DM, Wenzel RP. Cardiovascular surgery prophylaxis. A randomized, controlled comparison of cefazolin and cefuroxime. Journal of Thoracic and Cardiovascular Surgery. 1990;99(6):981-9.
- Galbraith U, Schilling J, Von Segesser LK, Carrel T, Turina M, Geroulanos S. Antibiotic prophylaxis in cardiovascular surgery: A prospective randomized comparative trial of one day cefazolin versus single dose cefuroxime. Drugs under Experimental and Clinical Research. 1993;19(5):229-34.
- Kaiser AB, Petracek MR, Lea 4th JW, Kernodle DS, Roach AC, Alford Jr WC, et al. Efficacy of cefazolin, cefamandole, and gentamicin as prophylactic agents in cardiac surgery. Results of a prospective, randomized, double-blind trial in 1030 patients. Annals of Surgery. 1987;206(6):791-7.
- Kreter B, Woods M. Antibiotic prophylaxis for cardiothoracic operations: Metaanalysis of thirty years of clinical trials. Journal of Thoracic and Cardiovascular Surgery. 1992;104(3):590-9.
- Slama TG, Sklar SJ, Misinski J, Fess SW. Randomized comparison of cefamandole, cefazolin, and cefuroxime prophylaxis in open-heart surgery. Antimicrobial agents and chemotherapy. 1986;29(5):744-7.
- Townsend TR, Reitz BA, Bilker WB, Bartlett JG. Clinical trial of cefamandole, cefazolin, and cefuroxime for antibiotic prophylaxis in cardiac operations. Journal of Thoracic and Cardiovascular Surgery. 1993;106(4):664-70.
- Wellens F, Pirlet M, Larbuisson R, De Meireleire F, De Somer P. Prophylaxis in cardiac surgery. A controlled randomized comparison between cefazolin and cefuroxime. European Journal of Cardio-thoracic Surgery. 1995;9(6):325-9.
- Baddour LM, Bettmann MA, Bolger AF, Epstein AE, Ferrieri P, Gerber MA, et al. Nonvalvular Cardiovascular Device-Related Infections. Circulation. 2003;108(16):2015-31.
- Bertaglia E, Zerbo F, Zardo S, Barzan D, Zoppo F, Pascotto P. Antibiotic prophylaxis with a single dose of cefazolin during pacemaker implantation: Incidence of long-term infective complications. PACE – Pacing and Clinical Electrophysiology. 2006;29(1):29-33.
- Boldt J, Piper S, Uphus D, Füssle R, Hempelmann G. Preoperative microbiologic screening and antibiotic prophylaxis in pulmonary resection operations. Annals of Thoracic Surgery. 1999;68(1):208-11.
- Schussler O, Dermine H, Alifano M, Casetta A, Coignard S, Roche N, et al. Should We Change Antibiotic Prophylaxis for Lung Surgery? Postoperative Pneumonia Is the Critical Issue. Annals of Thoracic Surgery. 2008;86(6):1727-33.
- Alerany C, Campany D, Monterde J, Semeraro C. Impact of local guidelines and an integrated dispensing system on antibiotic prophylaxis quality in a surgical centre. Journal of Hospital Infection. 2005;60(2):111-7.
- Imamura H, Furukawa H, Iijima S, Sugihara S, Tsujinaka T, Tsukuma H, et al. Multicenter phase II study of antimicrobial prophylaxis in low-risk patients undergoing distal gastrectomy for gastric cancer. Gastric Cancer. 2006;9(1):32-5.
- Kusachi S, Sumiyama Y, Nagao J, Arima Y, Yoshida Y, Tanaka H, et al. Prophylactic antibiotics given within 24 hours of surgery, compared with antibiotics given for 72 hours perioperatively, increased the rate of methicillin-resistant Staphylococcus aureus isolated from surgical site infections. Journal of Infection and Chemotherapy. 2008;14(1):44-50.
- Lewis RT. Discriminate use of antibiotic prophylaxis in gastroduodenal surgery. The American Journal of Surgery. 1979;138(5):640-3.
- Lewis RT, Allan CM, Goodall RG, Marien B, Park M, Lloyd-Smith W, et al. Cefamandole in gastroduodenal surgery: A controlled, prospective, randomized, double-blind study. Canadian Journal of Surgery. 1982;25(5):561-3.
- McArdle CS, Morran CG, Pettit L, Gemmell CG, Sleigh JD, Tillotson GS. Value of oral antibiotic prophylaxis in colorectal surgery. British Journal of Surgery. 1995;82(8):1046-8.
- Mitchell NJ, Evans DS, Pollock D. Pre-operation single-dose cefuroxime antimicrobial prophylaxis with and without metronidazole in elective gastrointestinal surgery. Journal of Antimicrobial Chemotherapy. 1980;6(3):393-9.
- Morris DL, Young D, Burdon DW, Keighley MRB. Prospective randomized trial of single dose cefuroxime against mezlocillin in elective gastric surgery. Journal of Hospital Infection. 1984;5(2):200-4.
- Nichols RL, Webb WR, Jones JW, Smith JW, LoCicero Iii J. Efficacy of antibiotic prophylaxis in high risk gastroduodenal operations. The American Journal of Surgery. 1982;143(1):94-8.
- Polk Jr HC, Lopez-Mayor JF. Postoperative wound infection: A prospective study of determinant factors and prevention. Surgery. 1969;66(1):97-103.
- Pories WJ, van Rij M, Burlingham BT, Fulghum RS, Meelheim D. Prophylactic cefazolin in gastric bypass surgery. Surgery. 1981;90(2):426-32.
- Radhakrishnan NV, Shenoy AH, Cartmill I, Sharma RK, George R, Foster DN, et al. Addition of local antiseptic spray to parenteral antibiotic regimen reduces the incidence of stomal infection following percutaneous endoscopic gastrostomy: A randomized controlled trial. European Journal of Gastroenterology and Hepatology. 2006;18(12):1279-84.
- Sharma VK, Howden CW. Meta-analysis of randomized, controlled trials of antibiotic prophylaxis before percutaneous endoscopic gastrostomy. American Journal of Gastroenterology. 2000;95(11):3133-6.
- Stone HH. Gastric surgery. Southern Medical Journal. 1977;70(10):35-7.
- Stone HH, Haney BB, Kolb LD, Geheber CE, Hooper CA. Prophylactic and preventive antibiotic therapy. Timing, duration and economics. Annals of Surgery. 1979;189(6):691-9.
- Sturgis TM, Yancy W, Cole JC, Proctor DD, Minhas BS, Marcuard SP. Antibiotic prophylaxis in percutaneous endoscopic gastrostomy. American Journal of Gastroenterology. 1996;91(11):2301-4.
- Ueno T, Yamamoto K, Kawaoka T, Takashima M, Oka M. Current antibiotic prophylaxis in pancreatoduodenectomy in Japan. Journal of Hepato-Biliary-Pancreatic Surgery. 2005;12(4):304-9.
- Agrawal CS, Sehgal R, Singh RK, Gupta AK. Antibiotic prophylaxis in elective cholecystectomy: A randomized, double blinded study comparing ciprofloxacin and cefuroxime. Indian Journal of Physiology and Pharmacology. 1999;43(4):501-4.
- Cainzos M, Sayek I, Wacha H, Pulay I, Dominion L, Aeberhard PF, et al. Septic complications after biliary tract stone surgery: A review and report of the European prospective study. Hepato-Gastroenterology. 1997;44(16):959-67.
- Chang WT, Lee KT, Chuang SC, Wang SN, Kuo KK, Chen JS, et al. The impact of prophylactic antibiotics on postoperative infection complication in elective laparoscopic cholecystectomy: a prospective randomized study. American journal of surgery. 2006;191(6):721-5.
- Crenshaw CA, Glanges E, Webber CE, McReynolds DB. A prospective, randomized, double blind study of preventive cefamandole therapy in patients at high risk for undergoing cholecystectomy. Surgery Gynecology and Obstetrics. 1981;153(4):546-52.
- Den Hoed PT, Boelhouwer RU, Veen HF, Hop WCJ, Bruining HA. Infections and bacteriological data after laparoscopic and open gallbladder surgery. Journal of Hospital Infection. 1998;39(1):27-37.
- Dobay KJ, Freier DT, Albear P. The absent role of prophylactic antibiotics in low-risk patients undergoing laparoscopic cholecystectomy. American Surgeon. 1999;65(3):226-8.
- Drumm J, Donovan IA, Wise R. A comparison of cefotetan and cephazolin for prophylaxis against wound infection after elective cholecystectomy. Journal of Hospital Infection. 1985;6(3):277-80.
- Garcia-Rodriguez JA, Puig-LaCalle J, Arnau C, Porta M, Vallvé C. Antibiotic prophylaxis with cefotaxime in gastroduodenal and biliary surgery. The American Journal of Surgery. 1989;158(5):428-32.
- Grant MD, Jones RC, Wilson SE, Bombeck CT, Flint LM, Jonasson O, et al. Single dose cephalosporin prophylaxis in high-risk patients undergoing surgical treatment of the biliary tract. Surgery Gynecology and Obstetrics. 1992;174(5):347-54.
- Harling R, Moorjani N, Perry C, MacGowan AP, Thompson MH. A prospective, randomised trial of prophylactic antibiotics versus bag extraction in the prophylaxis of wound infection in laparoscopic cholecystectomy. Annals of the Royal College of Surgeons of England. 2000;82(6):408-10.
- Higgins A, London J, Charland S, Ratzer E, Clark J, Haun W, et al. Prophylactic antibiotics for elective laparoscopic cholecystectomy: Are they necessary? Archives of Surgery. 1999;134(6):611-4.
- Illig KA, Schmidt E, Cavanaugh J, Krusch D, Sax HC. Are prophylactic antibiotics required for elective laparoscopic cholecystectomy? Journal of the American College of Surgeons. 1997;184(4):353-6.
- Jewesson PJ, Stiver G, Wai A, Frighetto L, Nickoloff D, Smith J, et al. Double-blind comparison of cefazolin and ceftizoxime for prophylaxis against infections following elective biliary tract surgery. Antimicrobial agents and chemotherapy. 1996;40(1):70-4.
- Kellum Jr JM, Gargano S, Gorbach SL, Talcof C, Curtis LE, Weiner B, et al. Antibiotic prophylaxis in high-risk biliary operations: Multicenter trial of single preoperative ceftriaxone versus multidose cefazolin. American journal of surgery. 1984;148(4 A):15-8.
- Krige JEJ, Isaacs S, Stapleton GN, McNally J. Prospective, randomized study comparing amoxycillin-clavulanic acid and cefamandole for the prevention of wound infection in high-risk patients undergoing elective biliary surgery. Journal of Hospital Infection. 1992;22(SUPPL. 1):33-41.
- Kujath P. Brief report: Antibiotic prophylaxis in biliary tract surgery. Ciprofloxacin versus ceftriaxone. The American Journal of Medicine. 1989;87(5 SUPPL. 1).
- Lapointe RW, Roy AF, Turgeon PL, Lewis RT, Dagenais MH, Joly JR, et al. Comparison of single-dose cefotetan and multidose cefoxitin as intravenous prophylaxis in elective, open biliary tract surgery: A multicentre, double-blind, randomized study. Canadian Journal of Surgery. 1994;37(4):313-8.
- Leaper DJ, Cooper MJ, Turner A. A comparative trial between cefotetan and cephazolin for wound sepsis prophylaxis during elective upper gastrointestinal surgery with an investigation of cefotetan penetration into the obstructed biliary tree. Journal of Hospital Infection. 1986;7(3):269-76.
- Lippert H, Gastinger J. Antimicrobial prophylaxis in laparoscopic and conventional cholecystectomy: Conclusions of a large prospective multicenter quality assurance study in Germany. Chemotherapy. 1998;44(5):355-63.
- Maki DG, Lammers JL, Aughey DR. Comparative studies of multiple-dose cefoxitin vs. single-dose cefonicid for surgical prophylaxis in patients undergoing biliary tract operations or hysterectomy. Reviews of Infectious Diseases. 1984;6 Suppl 4.
- McGuckin M, Shea JA, Schwartz JS. Infection and antimicrobial use in laparoscopic cholecystectomy. Infection control and hospital epidemiology. 1999;20(9):624-5.
- Meijer WS, Schmitz PIM. Prophylactic use of cefuroxime in biliary tract surgery: Randomized controlled trial of single versus multiple dose in high‐risk patients. British Journal of Surgery. 1993;80(7):917-21.
- Sirinek KR, Schauer PR, Yellin AE, Berne TV, Heseltine P, Appleman M, et al. Single-dose cefuroxime versus multiple-dose cefazolin as prophylactic therapy for high-risk cholecystectomy. Journal of the American College of Surgeons. 1994;178(4):321-5.
- Targarona EM, Garau J, Munoz-Ramos C, Roset F, Lite J, Matas E, et al. Single-dose antibiotic prophylaxis in patients at high risk for infection in biliary surgery: A prospective and randomized study comparing cefonicid with mezlocillin. Surgery. 1990;107(3):327-34.
- Tonelli F, Mazzei T, Novelli A, Mazzoni P, Ficari F. Amoxicillin/clavulanic acid versus cefotaxime for antimicrobial prophylaxis in abdominal surgery: A randomized trial. Journal of Chemotherapy. 2002;14(4):366-72.
- Choudhary A, Bechtold ML, Puli SR, Othman MO, Roy PK. Role of prophylactic antibiotics in laparoscopic cholecystectomy: A meta-analysis. Journal of Gastrointestinal Surgery. 2008;12(11):1847-53.
- Zhou H, Zhang J, Wang Q, Hu Z. Meta-analysis: Antibiotic prophylaxis in elective laparoscopic cholecystectomy. Alimentary Pharmacology and Therapeutics. 2009;29(10):1086-95.
- Guzmán-Valdivia G. Routine administration of antibiotics to patients suffering accidental gallbladder perforation during laparoscopic cholecystectomy is not necessary. Surgical Laparoscopy, Endoscopy and Percutaneous Techniques. 2008;18(6):547-50.
- Al-Dhohayan A, Al-Sebayl M, Shibl A, Al-Eshalwy S, Kattan K, Al-Saleh M. Comparative study of augmentin versus metronidazole/gentamicin in the prevention of infections after appendicectomy. European Surgical Research. 1993;25(1):60-4.
- Helmer KS, Robinson EK, Lally KP, Vasquez JC, Kwong KL, Liu TH, et al. Standardized patient care guidelines reduce infectious morbidity in appendectomy patients. American journal of surgery. 2002;183(6):608-13.
- Lau WY, Fan ST, Chu KW, Suen HC, Yiu TF, Wong KK. Randomized, prospective, and double-blind trial of new β-lactams in the treatment of appendicitis. Antimicrobial agents and chemotherapy. 1985;28(5):639-42.
- Lau WY, Fan ST, Chu KW, Yip WC, Yin TF, Yeung C, et al. Cefoxitin versus gentamicin and metronidazole in prevention of post-appendicectomy sepsis: A randomized, prospective trial. Journal of Antimicrobial Chemotherapy. 1986;18(5):613-9.
- Lau WY, Fan ST, Yiu TF, Poon GP, Wong SH. Prophylaxis of postappendicectomy sepsis by metronidazole and cefotaxime; a randomized, prospective and double blind trial. British Journal of Surgery. 1983;70(11):670-2.
- Lau WY, Fan ST, Yiu TF, Wong SH. Prophylaxis of post‐appendicectomy sepsis by metronidazole and ampicillin: A randomized, prospective and double‐blind trial. British Journal of Surgery. 1983;70(3):155-7.
- Liberman MA, Greason KL, Frame S, Ragland JJ. Single-dose cefotetan or cefoxitin versus multiple-dose cefoxitin as prophylaxis in patients undergoing appendectomy for acute nonperforated appendicitis. Journal of the American College of Surgeons. 1995;180(1):77-80.
- Morris DL, Wilson SR, Pain J, Edwardson KF, Jones J, Strachan C, et al. A comparison of aztreonam/metronidazole and cefotaxime/metronidazole in elective colorectal surgery: Antimicrobial prophylaxis must include gram-positive cover. Journal of Antimicrobial Chemotherapy. 1990;25(4):673-8.
- Morris WT, Innes DB, Richardson RA, Lee AJ, Ellis‐Pegler RB. THE PREVENTION OF POST‐APPENDICECTOMY SEPSIS BY METRONIDAZOLE AND CEFAZOLIN: A CONTROLLED DOUBLE BLIND TRIAL. Australian and New Zealand Journal of Surgery. 1980;50(4):429-33.
- O’Rourke MGE, Wynne JM, Morahan RJ, Green AJ, Walker RM, Wilson ME. PROPHYLACTIC ANTIBIOTICS IN APPENDICECTOMY: A PROSPECTIVE DOUBLE BLIND RANDOMIZED STUDY. Australian and New Zealand Journal of Surgery. 1984;54(6):535-41.
- Salam IMA, Galala KHA, El Ashaal YI, Chandran VPP, Asham NN, Sim AJW. A randomized prospective study of cefoxitin versus piperacillin in appendicectomy. Journal of Hospital Infection. 1994;26(2):133-6.
- Winslow RE, Dean RE, Harley JW. Acute Nonperforating Appendicitis: Efficacy of Brief Antibiotic Prophylaxis. Archives of Surgery. 1983;118(5):651-5.
- Múñez E, Ramos A, Espejo TTD, Vaqué J, Sánchez-Payá J, Pastor V, et al. Microbiology of surgical site infections in abdominal tract surgery patients. Cirugia Espanola. 2011;89(9):606-12.
- Sanchez-Manuel FJ, Lozano-García J, Seco-Gil JL. Antibiotic prophylaxis for hernia repair. Cochrane database of systematic reviews (Online). 2012;2.
- Yin Y, Song T, Liao B, Luo Q, Zhou Z. Antibiotic prophylaxis in patients undergoing open mesh repair of inguinal hernia: A meta-analysis. American Surgeon. 2012;78(3):359-65.
- AhChong K, Yip AWC, Lee FCW, Chiu KM. Comparison of prophylactic ampicillin/sulbactam with gentamicin and metronidazole in elective colorectal surgery: A randomized clinical study. Journal of Hospital Infection. 1994;27(2):149-54.
- Arnaud JP, Bellissant E, Boissel P, Carlet J, Chastang C, Lafaix C, et al. Single-dose amoxycillin-clavulanic acid vs.cefotetan for prophylaxis in elective colorectal surgery: a multicentre, prospective, randomized study. Journal of Hospital Infection. 1992;22(SUPPL. 1):23-32.
- Condon RE, Bartlett JG, Nichols RL, Schulte WJ, Gorbach SL, Ochi S. Preoperative prophylactic cephalothin fails to control septic complications of colorectal operations: Results of controlled clinical trial. A veterans administration cooperative study. The American Journal of Surgery. 1979;137(1):68-74.
- Hakansson T, Raahave D, Hart Hansen O, Pedersen T. Effectiveness of single dose prophylaxis with cefotaxime and metronidazole compared with three doses of cefotaxime alone in elective colorectal surgery. European Journal of Surgery, Acta Chirurgica. 1993;159(4):177-80.
- Hoffmann CEJ, McDonald PJ, Watts McK J. Use of peroperative Cefoxitin® to prevent infection after colonic and rectal surgery. Annals of Surgery. 1981;193(3):353-6.
- Itani KMF, Wilson SE, Awad SS, Jensen EH, Finn TS, Abramson MA. Ertapenem versus cefotetan prophylaxis in elective colorectal surgery. New England Journal of Medicine. 2006;355(25):2640-51.
- Jagelman DG, Fabian TC, Nichols RL, Stone HH, Wilson SE, Zellner SR. Single-dose cefotetan versus multiple-dose cefoxitin as prophylaxis in colorectal surgery. The American Journal of Surgery. 1988;155(5 SUPPL.):71-6.
- Jones RN, Wojeski W, Bakke J, Porter C, Searles M. Antibiotic prophylaxis of 1,036 patients undergoing elective surgical procedures. A prospective, randomized comparative trial of cefazolin, cefoxitin, and cefotaxime in a prepaid medical practice. The American Journal of Surgery. 1987;153(4):341-6.
- Kaiser AB, Herrington Jr JL, Jacobs JK, Mulherin Jr JL, Roach AC, Sawyers JL. Cefoxitin versus erythromycin, neomycin, and cefazolin in colorectal operations. Importance of the duration of the surgical procedure. Annals of Surgery. 1983;198(4):525-30.
- Karran SJ, Sutton G, Gartell P, Karran SE, Finnis D, Blenkinsop J. Imipenem prophylaxis in elective colorectal surgery. British Journal of Surgery. 1993;80(9):1196-8.
- Keighley MRB, Arabi Y, Alexander-Williams J, Youngs D, Burdon DW. COMPARISON BETWEEN SYSTEMIC AND ORAL ANTIMICROBIAL PROPHYLAXIS IN COLORECTAL SURGERY. The Lancet. 1979;313(8122):894-7.
- Kwok SPY, Lau WY, Leung KL, Ku KW, Ho WS, Li AKC. Amoxycillin and clavulanic acid versus cefotaxime and metronidazole as antibiotic prophylaxis in elective colorectal resectional surgery. Chemotherapy. 1993;39(2):135-9.
- Lewis RT, Allan CM, Goodall RG, Marien B, Park M, Lloyd-Smith W, et al. Are first-generation cephalosporins effective for antibiotic prophylaxis in elective surgery of the colony? Canadian Journal of Surgery. 1983;26(6):504-7.
- Lumley JW, Siu SK, Rllay SP, Stitz R, Kemp RJ, Faoagali J, et al. SINGLE DOSE CEFTRIAXONE AS PROPHYLAXIS FOR SEPSIS IN COLORECTAL SURGERY. Australian and New Zealand Journal of Surgery. 1992;62(4):292-6.
- McDermott FT, Polglase AL, Johnson WR, Hughes ESR. PREVENTION OF WOUND INFECTION IN ELECTIVE COLORECTAL RESECTIONS BY PREOPERATIVE CEPHAZOLIN WITH AND WITHOUT METRONIDAZOLE. Australian and New Zealand Journal of Surgery. 1981;51(4):351-3.
- Morton AL, Taylor EW, Lindsay G, Wells GR. A multicenter study to compare cefotetan alone with cefotetan and metronidazole as prophylaxis against infection in elective colorectal operations. Surgery Gynecology and Obstetrics. 1989;169(1):41-5.
- Periti P, Mazzei T, Tonelli F. Single-dose cefotetan vs. Multiple-dose cefoxitin-Antimicrobial prophylaxis in colorectal surgery – Results of a prospective, multicenter, randomized study. Diseases of the Colon & Rectum. 1989;32(2):121-7.
- Periti P, Tonelli F, Mazzei T, Ficari F. Antimicrobial chemoimmunoprophylaxis in colorectal surgery with cefotetan and thymostimulin: Prospective, controlled multicenter study. Journal of Chemotherapy. 1993;5(1):37-42.
- Sexton DJ. Carbapenems for surgical prophylaxis? New England Journal of Medicine. 2006;355(25):2693-5.
- Shatney CH. Antibiotic prophylaxis in elective gastro-intestinal tract surgery: A comparison of single-dose pre-operative cefotaxime and multiple-dose cefoxitin. Journal of Antimicrobial Chemotherapy. 1984;14(SUPPL. B):241-5.
- Skipper D, Karran SJ. A randomized prospective study to compare cefotetan with cefuroxime plus metronidazole as prophylaxis in elective colorectal surgery. Journal of Hospital Infection. 1992;21(1):73-7.
- Weaver M, Burdon DW, Youngs DJ, Keighley MRB. Oral neomycin and erythromycin compared with single-dose systemic metronidazole and ceftriaxone prophylaxis in elective colorectal surgery. The American Journal of Surgery. 1986;151(4):437-42.
- Zelenitsky SA, Silverman RE, Duckworth H, Harding GKM. A prospective, randomized, double-blind study of single high dose versus multiple standard dose gentamicin both in combination with metronidazole for colorectal surgical prophylaxis. Journal of Hospital Infection. 2000;46(2):135-40.
- Mangram AJ. Guideline for prevention of surgical site infection, 1999. Infection control and hospital epidemiology. 1999;20(4):250-78.
- Johnson JT, Kachman K, Wagner RL, Myers EN. Comparison of ampicillin/sulbactam versus clindamycin in the prevention of infection in patients undergoing head and neck surgery. Head and Neck. 1997;19(5):367-71.
- Johnson JT, Myers EN, Thearle PB, Sigler BA, Schramm VL. Antimicrobial prophylaxis for contaminated head and neck surgery. The Laryngoscope. 1984;94(1):46-51.
- SkitareliĆ N, MoroviĆ M, Manestar D. Antibiotic prophylaxis in clean-contaminated head and neck oncological surgery. Journal of Cranio-Maxillofacial Surgery. 2007;35(1):15-20.
- Weber RS, Raad I, Frankenthaler R, Hankins P, Byers RM, Guillamondegui O, et al. Ampicillin-Sulbactam vs Clindamycin in Head and Neck Oncologic Surgery: The Need for Gram-negative Coverage. Archives of Otolaryngology–Head and Neck Surgery. 1992;118(11):1159-63.
- Barker Ii FG. Efficacy of prophylactic antibiotics against meningitis after craniotomy: A meta-analysis. Neurosurgery. 2007;60(5):887-94.
- Korinek AM. Risk factors for neurosurgical site infections after craniotorny: A prospective multicenter study of 2944 patients. Neurosurgery. 1997;41(5):1073-81.
- Korinek AM, Baugnon T, Golmard JL, Van Effenterre R, Coriat P, Puybasset L. Risk factors for adult nosocomial meningitis after craniotomy: Role of antibiotic prophylaxis. Neurosurgery. 2006;59(1):126-32.
- Korinek AM, Golmard JL, Elcheick A, Bismuth R, Van Effenterre R, Coriat P, et al. Risk factors for neurosurgical site infections after craniotomy: A critical reappraisal of antibiotic prophylaxis on 4578 patients. British Journal of Neurosurgery. 2005;19(2):155-62.
- Whitby M, Johnson BC, Atkinson RL, Stuart G. The comparative efficacy of intravenous cefotaxime and trimethoprim/sulfamethoxazole in preventing infection after neurosurgery: A prospective, randomized study. British Journal of Neurosurgery. 2000;14(1):13-8.
- . AAP Comittee on Fetus and Newborn, ACOG Committee on Obstetric Practice. 2008.
- Andrews WW, Hauth JC, Cliver SP, Savage K, Goldenberg RL. Randomized clinical trial of extended spectrum antibiotic prophylaxis with coverage for Ureaplasma urealyticum to reduce post-cesarean delivery endometritis. Obstetrics and gynecology. 2003;101(6):1183-9.
- Hopkins L, Smaill F. Antibiotic prophylaxis regimens and drugs for cesarean section. Cochrane database of systematic reviews (Online). 2000(2).
- Meyer NL, Hosier KV, Scott K, Lipscomb GH. Cefazolin versus Cefazolin plus Metronidazole for Antibiotic Prophylaxis at Cesarean Section. Southern Medical Journal. 2003;96(10):992-5.
- Tita ATN, Hauth JC, Grimes A, Owen J, Stamm AM, Andrews WW. Decreasing incidence of postcesarean endometritis with extended-spectrum antibiotic prophylaxis. Obstetrics and gynecology. 2008;111(1):51-6.
- Tita ATN, Owen J, Stamm AM, Grimes A, Hauth JC, Andrews WW. Impact of extended-spectrum antibiotic prophylaxis on incidence of postcesarean surgical wound infection. American journal of obstetrics and gynecology. 2008;199(3).
- Berkeley AS, Freedman KS, Ledger WJ, Orr JW, Benigno BB, Gordon SF, et al. Comparison of cefotetan and cefoxitin prophylaxis for abdominal and vaginal hysterectomy. American journal of obstetrics and gynecology. 1988;158(3 II SUPPL.):706-9.
- Berkeley AS, Hayworth SD, Hirsch JC, Freedman KS, Ledger WJ. Controlled, comparative study of moxalactam and cefazolin for prophylaxis of abdominal hysterectomy. Surgery Gynecology and Obstetrics. 1985;161(5):457-61.
- Campillo F, Rubio JM. Comparative study of single-dose cefotaxime and multiple doses of cefoxitin and cefazolin as prophylaxis in gynecologic surgery. The American Journal of Surgery. 1992;164(4 SUPPL.).
- Chongsomchai C, Lumbiganon P, Thinkhamrop J, Ounchai J, Vudhikamraksa N. Placebo-controlled, double-blind, randomized study of prophylactic antibiotics in elective abdominal hysterectomy. Journal of Hospital Infection. 2002;52(4):302-6.
- Gordon SF. Results of a single-center study of cefotetan prophylaxis in abdominal or vaginal hysterectomy. American journal of obstetrics and gynecology. 1988;158(3 II SUPPL.):710-4.
- Hemsell DL, Heard ML, Nobles BJ, Hemsell PG. Single-Dose cefoxitin prophylaxis for premenopausal women undergoing vaginal hysterectomy. Obstetrics and gynecology. 1984;63(3):285-90.
- Hemsell DL, Johnson ER, Bawdon RE, Nobles BJ, Heard ML. Ceftriaxone and cefazolin prophylaxis for hysterectomy. Surgery Gynecology and Obstetrics. 1985;161(3):197-203.
- Hemsell DL, Johnson ER, Hemsell PG, Nobles BJ, Little BB, Heard MC. Cefazolin is inferior to cefotetan as single-dose prophylaxis for women undergoing elective total abdominal hysterectomy. Clinical Infectious Diseases. 1995;20(3):677-84.
- Hemsell DL, Menon MO, Friedman AJ. Ceftriaxone or cefazolin prophylaxis for the prevention of infection after vaginal hysterectomy. American journal of surgery. 1984;148(4 A):22-6.
- McGregor JA, Phillips LE, Roy S, Dunne JT, Warwaruk AS, Johnston DW, et al. Results of a double-blind, placebo-controlled clinical trial program of single-dose ceftizoxime versus multiple-dose cefoxitin as prophylaxis for patients undergoing vaginal and abdominal hysterectomy. Journal of the American College of Surgeons. 1994;178(2):123-31.
- Mercer LJ, Murphy HJ, Ismail MA, Hajj SN. A comparison of cefonicid and cefoxitin for preventing infections after vaginal hysterectomy. Journal of Reproductive Medicine for the Obstetrician and Gynecologist. 1988;33(2):223-6.
- Orr Jr JW, Varner RE, Kilgore LC, Holloway RC, McDiarmid M. Cefotetan versus cefoxitin as prophylaxis in hysterectomy. American journal of obstetrics and gynecology. 1986;154(4):960-3.
- Orr JW, Sisson PF, Barrett JM, Ellington JR, Jennings RH, Taylor DL. Single-center study results of cefotetan and cefoxitin prophylaxis for abdominal or vaginal hysterectomy. American journal of obstetrics and gynecology. 1988;158(3 II SUPPL.):714-6.
- Rapp RP, Connors JE, Hager WD, Donaldson ES, van Nagell Jr JR. Comparison of single-dose moxalactam and a three-dose regimen of cefoxitin for prophylaxis in vaginal hysterectomy. Clinical Pharmacy. 1986;5(12):988-93.
- Roy S, Wilkins J. Single-dose cefotaxime versus 3 to 5 dose cefoxitin for prophylaxis of vaginal or abdominal hysterectomy. Journal of Antimicrobial Chemotherapy. 1984;14(SUPPL. B):217-21.
- Roy S, Wilkins J, Galaif E, Azen C. Comparative efficacy and safety of cefmetazole or cefoxitin in the prevention of postoperative infection following vaginal and abdominal hysterectomy. Journal of Antimicrobial Chemotherapy. 1989;23(SUPPL. D):109-17.
- Roy S, Wilkins J, Hemsell DL, March CM, Spirtos NM. Efficacy and safety of single-dose ceftizoxime vs. multiple-dose cefoxitin in preventing infection after vaginal hysterectomy. Journal of Reproductive Medicine for the Obstetrician and Gynecologist. 1988;33(1 SUPPL.):149-53.
- Tuomala RE, Fischer SG, Muñoz A, Souney PF, Steele L, Frank Polk B. A comparative trial of cefazolin and moxalactam as prophylaxis for preventing infection after abdominal hysterectomy. Obstetrics and gynecology. 1985;66(3):372-6.
- Barequet IS, Jabbur NS, Barron Y, Osterhout GJ, O’Brien TP. Perioperative microbiologic profile of the conjunctiva in photorefractive keratectomy. Journal of Refractive Surgery. 2001;17(1):55-62.
- Fernández-Rubio E, Urcelay JL, Cuesta-Rodriguez T. The antibiotic resistance pattern of conjunctival bacteria: A key for designing a cataract surgery prophylaxis. Eye. 2009;23(6):1321-8.
- Osher RH, Amdahl LD, Cheetham JK. Antimicrobial efficacy and aqueous humor concentration of preoperative and postoperative topical trimethoprim/polymyxin B sulfate versus tobramycin. Journal of cataract and refractive surgery. 1994;20(1):3-8.
- Park SH, Lim JA, Choi JS, Kim KA, Joo CK. The resistance patterns of normal ocular bacterial flora to 4 fluoroquinolone antibiotics. Cornea. 2009;28(1):68-72.
- Recchia FM, Busbee BG, Pearlman RB, Carvalho-Recchia CA, Ho AC. Changing trends in the microbiologic aspects of postcataract endophthalmitis. Archives of Ophthalmology. 2005;123(3):341-6.
- Bucci Jr FA. An in vivo study comparing the ocular absorption of levofloxacin and ciprofloxacin prior to phacoemulsification. American Journal of Ophthalmology. 2004;137(2):308-12.
- Cahane M, Ben Simon GJ, Barequet IS, Grinbaum A, Diamanstein-Weiss L, Goller O, et al. Human corneal stromal tissue concentration after consecutive doses of topically applied 3.3% vancomycin. British Journal of Ophthalmology. 2004;88(1):22-4.
- Chisari G, Cavallaro G, Reibaldi M, Biondi S. Presurgical antimicrobial prophylaxis: Effect on ocular flora in healthy patients. International Journal of Clinical Pharmacology and Therapeutics. 2004;42(1):35-8.
- Moshirfar M, Feiz V, Vitale AT, Wegelin JA, Basavanthappa S, Wolsey DH. Endophthalmitis after Uncomplicated Cataract Surgery with the Use of Fourth-Generation Fluoroquinolones. A Retrospective Observational Case Series. Ophthalmology. 2007;114(4):686-91.
- Pavel A, Smith RL, Ballard A, Larsen IJ. Prophylactic antibiotics in clean orthopaedic surgery. Journal of Bone and Joint Surgery – Series A. 1974;56(4):777-82.
- Prokuski L. Prophylactic antibiotics in orthopaedic surgery. Journal of the American Academy of Orthopaedic Surgeons. 2008;16(5):283-93.
- Zgonis T, Jolly GP, Garbalosa JC. The efficacy of prophylactic intravenous antibiotics in elective foot and ankle surgery. Journal of Foot and Ankle Surgery. 2004;43(2):97-103.
- Barker Ii FG, McCormick PC, Haines SJ, Benzel EC. Efficacy of prophylactic antibiotic therapy in spinal surgery: A meta-analysis. Neurosurgery. 2002;51(2):391-401.
- Hellbusch LC, Helzer-Julin M, Doran SE, Leibrock LG, Long DJ, Puccioni MJ, et al. Single-dose vs multiple-dose antibiotic prophylaxis in instrumented lumbar fusion-a prospective study. Surgical Neurology. 2008;70(6):622-7.
- Rimoldi RL, Haye W. The use of antibiotics for wound prophylaxis in spinal surgery. Orthopedic Clinics of North America. 1996;27(1):47-52.
- Walters R, Moore R, Fraser R. Penetration of cephazolin in human lumbar intervertebral disc. Spine. 2006;31(5):567-70.
- Watters Iii WC, Baisden J, Bono CM, Heggeness MH, Resnick DK, Shaffer WO, et al. Antibiotic prophylaxis in spine surgery: an evidence-based clinical guideline for the use of prophylactic antibiotics in spine surgery. Spine Journal. 2009;9(2):142-6.
- . Information Statement: The use of Prophylactic Antibiotics in Orthopaedic Medicine and the Emergence of Vancomycin-resistant Bacteria. 0000.
- Cunha BA, Gossling HR, Pasternak HS, Nightingale CH, Quintiliani R. The penetration characteristics of cefazolin, cephalothin, and cephradine into bone in patients undergoing total hip replacement. Journal of Bone and Joint Surgery – Series A. 1977;59(7):856-9.
- Gulihar A, Nixon M, Jenkins D, Taylor GJS. Clostridium difficile in hip fracture patients: Prevention, treatment and associated mortality. Injury. 2009;40(7):746-51.
- Southwell-Keely JP, Russo RR, March L, Cumming R, Cameron I, Brnabic AJM. Antibiotic Prophylaxis in Hip Fracture Surgery: A Metaanalysis. Clinical orthopaedics and related research. 2004(419):179-84.
- Starks I, Ayub G, Walley G, Orendi J, Roberts P, Maffulli N. Single-dose cefuroxime with gentamicin reduces Clostridium difficile-associated disease in hip-fracture patients. Journal of Hospital Infection. 2008;70(1):21-6.
- AlBuhairn B, Hind D, Hutchinson A. Antibiotic prophylaxis for wound infections in total joint arthroplasty : A systematic review. Journal of Bone and Joint Surgery – Series B. 2008;90(7):915-9.
- Josefsson G, Kolmert L. Prophylaxis with systematic antibiotics versus gentamicin bone cement in total hip arthroplasty: A ten-year survey of 1688 hips. Clinical orthopaedics and related research. 1993(292):210-4.
- McQueen MM, Hughes SPF, May P, Verity L. Cefuroxime in total joint arthroplasty: Intravenous or in bone cement. Journal of Arthroplasty. 1990;5(2):169-72.
- Berry A, Barratt A. Prophylatic antibiotic use in transurethral prostatic resection: A meta-analysis. Journal of Urology. 2002;167(2 I):571-7.
- Ferguson KH, Mc Neil JJ, Morey AF. Mechanical and antibiotic bowel preparation for urinary diversion surgery. Journal of Urology. 2002;167(6):2352-6.
- Wagenlehner FME, Wagenlehner C, Schinzel S, Naber KG, Bach D, Basting R, et al. Prospective, randomized, multicentric, open, comparative study on the efficacy of a prophylactic single dose of 500 mg levofloxacin versus 1920 mg trimethoprim/sulfamethoxazole versus a control group in patients undergoing TUR of the prostate. European urology. 2005;47(4):549-56.
- Hoffelt SC, Wallner K, Merrick G. Epididymitis after prostate brachytherapy. Urology. 2004;63(2):293-6.
- Johnson MI, Merrilees D, Robson WA, Lennon T, Masters J, Orr KE, et al. Oral ciprofloxacin or trimethoprim reduces bacteriuria after flexible cystoscopy. BJU international. 2007;100(4):826-9.
- Latthe PM, Foon R, Toozs-Hobson P. Prophylactic antibiotics in urodynamics: A systematic review of effectiveness and safety. Neurourology and Urodynamics. 2008;27(3):167-73.
- Bhatia NN, Karram MM, Bergman A. Role of antibiotic prophylaxis in retropubic surgery for stress urinary incontinence. Obstetrics and gynecology. 1989;74(4):637-9.
- Brewster SF, Macgowan AP, Gingell JC. Antimicrobial prophylaxis for transrectal prostatic biopsy: a prospective randomized trial of cefuroxime versus piperacillin/tazobactam. British Journal of Urology. 1995;76(3):351-4.
- Christiano AP, Hollowell CMP, Kim H, Kim J, Patel R, Bales GT, et al. Double-blind randomized comparison of single-dose ciprofloxacin versus intravenous cefazolin in patients undergoing outpatient endourologic surgery. Urology. 2000;55(2):182-5.
- Cormio L, Berardi B, Callea A, Fiorentino N, Sblendorio D, Zizzi V, et al. Antimicrobial prophylaxis for transrectal prostatic biopsy: A prospective study of ciprofloxacin vs piperacillin/tazobactam. BJU international. 2002;90(7):700-2.
- Gibbons RP, Stark RA, Correa Jr RJ, Cummings KB, Mason JT. The prophylactic use – or misuse – of antibiotics in transurethral prostatectomy. Journal of Urology. 1978;119(3):381-3.
- Gombert ME, Dubouchet L, Aulicino TM, Berkowitz LB, Macchia RJ. Brief report: Intravenous ciprofloxacin versus cefotaxime prophylaxis during transurethral surgery. The American Journal of Medicine. 1989;87(5 SUPPL. 1).
- Grabe M, Bjerklund-Johansen TE, Botto H. Guidelines on Urological Infections. Guidelines on Urological Infections. 2013.
- Hills NH, Bultitude MI, Eykyn S. Co-trimoxazole in prevention of bacteriuria after prostatectomy. British Medical Journal. 1976;2(6034):498-9.
- Klimberg IW, Malek GH, Cox CE, Patterson AL, Whalen E, Kowalsky SF, et al. Single-dose oral ciprofloxacin compared with cefotaxime and placebo for prophylaxis during transurethral surgery. Journal of Antimicrobial Chemotherapy. 1999;43(SUPPL. A):77-84.
- Ramsey EW, Sheth NK. Antibiotic prophylaxis in patients undergoing prostatectomy. Urology. 1983;21(4):376-8.
- Sakura M, Kawakami S, Yoshida S, Masuda H, Kobayashi T, Kihara K. Prospective comparative study of single dose versus 3-day administration of antimicrobial prophylaxis in minimum incision endoscopic radical prostatectomy. International Journal of Urology. 2008;15(4):328-31.
- Terai A, Ichioka K, Kohei N, Ueda N, Utsunomiya N, Inoue K. Antibiotic prophylaxis in radical prostatectomy: 1-Day versus 4-day treatments. International Journal of Urology. 2006;13(12):1488-93.
- Yamamoto S, Kanamaru S, Kunishima Y, Ichiyama S, Ogawa O. Perioperative antimicrobial prophylaxis in urology: A multi-center prospective study. Journal of Chemotherapy. 2005;17(2):189-97.
- Bratzler DW, Houck PM. Antimicrobial prophylaxis for surgery: An advisory statement from the national surgical infection prevention project. Clinical Infectious Diseases. 2004;38(12):1706-15.
- Edwards Jr WH, Kaiser AB, Kernodle DS, Appleby TC, Edwards Sr WH, Martin Iii RS, et al. Cefuroxime versus cefazolin as prophylaxis in vascular surgery. Journal of Vascular Surgery. 1992;15(1):35-42.
- Edwards Jr WH, Kaiser AB, Tapper S, Edwards Sr WH, Martin Iii RS, Mulherin Jr JL, et al. Cefamandole versus cefazolin in vascular surgical wound infection prophylaxis: Cost-effectiveness and risk factors. Journal of Vascular Surgery. 1993;18(3):470-6.
- Murray BE. Problems and dilemmas of antimicrobial resistance. Pharmacotherapy. 1992;12(6 II).
- Risberg B, Drott C, Dalman P, Holm J, Ivarsson L, Jivegård L, et al. Oral ciprofloxacin versus intravenous cefuroxime as prophylaxis against postoperative infection in vascular surgery: A randomised double-blind, prospective multicentre study. European Journal of Vascular and Endovascular Surgery. 1995;10(3):346-51.
- Ross CB, Wheeler Ii WG, Jones MJ, Kerins CA, Peek TE. Ceftriaxone versus cefazolin in peripheral arterial operations: A randomized, prospective trial. Southern Medical Journal. 1997;90(1):16-22.
- Carrier M, Perrault LP, Pellerin M, Marchand R, Auger P, Pelletier GB, et al. Sternal wound infection after heart transplantation: Incidence and results with aggressive surgical treatment. Annals of Thoracic Surgery. 2001;72(3):719-23.
- Filsoufi F, Rahmanian PB, Castillo JG, Pinney S, Broumand SR, Adams DH. Incidence, Treatment Strategies and Outcome of Deep Sternal Wound Infection After Orthotopic Heart Transplantation. Journal of Heart and Lung Transplantation. 2007;26(11):1084-90.
- Kaiser AB. Use of antibiotics in cardiac and thoracic surgery. Surgery of the Chest. 1995:98-116.
- Muñoz P, Menasalvas A, Bernaldo De Quirós JCL, Desco M, Vallejo JL, Bouza E. Postsurgical mediastinitis: A case-control study. Clinical Infectious Diseases. 1997;25(5):1060-4.
- Ramos A, Asensio A, Muñez E, Torre-Cisneros J, Blanes M, Carratalá J, et al. Incisional surgical infection in heart transplantation. Transplant Infectious Disease. 2008;10(4):298-302.
- Abid Q, Nkere UU, Hasan A, Gould K, Forty J, Corris P, et al. Mediastinitis in heart and lung transplantation: 15 Years experience. Annals of Thoracic Surgery. 2003;75(5):1565-71.
- Campos S, Caramori M, Teixeira R, Afonso Jr J, Carraro R, Strabelli T, et al. Bacterial and Fungal Pneumonias After Lung Transplantation. Transplantation Proceedings. 2008;40(3):822-4.
- Fishman JA. Infection in solid-organ transplant recipients. New England Journal of Medicine. 2007;357(25):2601-14.
- Mattner F, Kola A, Fischer S, Becker T, Haverich A, Simon A, et al. Impact of bacterial and fungal donor organ contamination in lung, heart-lung, heart and liver transplantation. Infection. 2008;36(3):207-12.
- Soave R. Prophylaxis strategies for solid-organ transplantation. Clinical Infectious Diseases. 2001;33(SUPPL. 1).
- Trulock EP. Lung transplantation. American Journal of Respiratory and Critical Care Medicine. 1997;155(3):789-818.
- Arnow PM, Carandang GC, Zabner R, Irwin ME. Randomized controlled trial of selective bowel decontamination for prevention of infections following liver transplantation. Clinical Infectious Diseases. 1996;22(6):997-1003.
- Arnow PM, Zachary KC, Thistlethwaite JR, Thompson KD, Bova JL, Newell KA. Pathogenesis of early operative site infections after orthotopic liver transplantation. Transplantation. 1998;65(11):1500-3.
- Asensio A, Ramos A, Cuervas-Mons V, Cordero E, Sánchez-Turrión V, Blanes M, et al. Effect of antibiotic prophylaxis on the risk of surgical site infection in orthotopic liver transplant. Liver Transplantation. 2008;14(6):799-805.
- Barkholt LM, Andersson J, Ericzon BG, Palmgren AC, Broomé U, Duraj F, et al. Stool cultures obtained before liver transplantation are useful for choice of perioperative antibiotic: Prophylaxis. Transplant International. 1997;10(6):432-8.
- Bedini A, Codeluppi M, Cocchi S, Guaraldi G, Di Benedetto F, Venturelli C, et al. Gram-Positive Bloodstream Infections in Liver Transplant Recipients: Incidence, Risk Factors, and Impact on Survival. Transplantation Proceedings. 2007;39(6):1947-9.
- Bion JF, Badger I, Crosby HA, Hutchings P, Kong KL, Baker J, et al. Selective decontamination of the digestive tract reduces gram-negative pulmonary colonization but not systemic endotoxemia in patients undergoing elective liver transplantation. Critical care medicine. 1994;22(1):40-9.
- Chang FY, Singh N, Gayowski T, Drenning SD, Wagener MM, Marino IR. Staphylococcus aureus nasal colonization and association with infections in liver transplant recipients. Transplantation. 1998;65(9):1169-72.
- Colonna JO, Winston DJ, Brill JE, Goldstein LI, Hoff MP, Hiatt JR, et al. Infectious Complications in Liver Transplantation. Archives of Surgery. 1988;123(3):360-4.
- García Prado ME, Matia EC, Ciuro FP, Díez-Canedo JS, Sousa Martín JM, Porras López FM, et al. Surgical site infection in liver transplant recipients: Impact of the type of perioperative prophylaxis. Transplantation. 2008;85(12):1849-54.
- Kim YJ, Kim SI, Wie SH, Kim YR, Hur JA, Choi JY, et al. Infectious complications in living-donor liver transplant recipients: A 9-year single-center experience. Transplant Infectious Disease. 2008;10(5):316-24.
- Kuo PC, Bartlett ST, Lim JW, Plotkin JS, Wilson S, Johnson LB. Selective bowel decontamination in hospitalized patients awaiting liver transplantation. American journal of surgery. 1997;174(6):745-9.
- Kusne S, Stephen Dummer J, Singh N, Iwatsuki S, Makowka L, Esquivel C, et al. Infections after liver transplantation: An analysis of 101 consecutive cases. Medicine (United States). 1988;67(2):132-43.
- Singh N, Paterson DL, Gayowski T, Wagener MM, Marino IR. Predicting bacteremia and bacteremic mortality in liver transplant recipients. Liver Transplantation. 2000;6(1):54-61.
- Uemoto S, Tanaka K, Fujita S, Sano K, Shirahase I, Kato H, et al. Infectious complications in living related liver transplantation. Journal of Pediatric Surgery. 1994;29(4):514-7.
- Zwaveling JH, Maring JK, Klompmaker IJ, Haagsma EB, Bottema JT, Laseur M, et al. Selective decontamination of the digestive tract to prevent postoperative infection: A randomized placebo-controlled trial in liver transplant patients. Critical Care Medicine. 2002;30(6):1204-9.
- Bassetti M, Salvalaggio PRO, Topal J, Lorber MI, Friedman AL, Andriole VT, et al. Incidence, timing and site of infections among pancreas transplant recipients. Journal of Hospital Infection. 2004;56(3):184-90.
- Douzdjian V, Gugliuzza KK. Wound complications after simultaneous pancreas-kidney transplants: Midline versus transverse incision. Transplantation Proceedings. 1995;27(6):3130-2.
- Everett JE, Wahoff DC, Statz C, Gillingham KJ, Gruessner A, Gruessner RWG, et al. Characterization and Impact of Wound Infection After Pancreas Transplantation. Archives of Surgery. 1994;129(12):1310-7.
- Freise CE, Stock PG, Roberts JP, Melzer JS. Low postoperative wound infection rates are possible following simultaneous pancreas-kidney transplantation. Transplantation Proceedings. 1995;27(6):3069-70.
- Linhares MM, Gonzalez AM, Triviño T, Barbosa MMLS, Schraibman V, Melaragno C, et al. Simultaneous pancreas-kidney transplantation: Infectious complications and microbiological aspects. Transplantation Proceedings. 2004;36(4):980-1.
- Michalak G, Kwiatkowski A, Bieniasz M, Meszaros J, Czerwinski J, Wszola M, et al. Infectious complications after simultaneous pancreas-kidney transplantation. Transplantation Proceedings. 2005;37(8):3560-3.
- Capocasale E, Mazzoni MP, Tondo S, D’Errico G. Antimicrobial prophylaxis with ceftriaxone in renal transplantation: Prospective study of 170 patients. Chemotherapy. 1994;40(6):435-40.
- Cohen J, Rees AJ, Williams G. A prospective randomized controlled trial of perioperative antibiotic prophylaxis in renal transplantation. Journal of Hospital Infection. 1988;11(4):357-63.
- Del Rio G, Dalet F, Chechile G, Naber KG. Antimicrobial prophylaxis in urologic surgery: Does it give some benefit? European urology. 1993;24(3):305-12.
- Judson RT. WOUND INFECTION FOLLOWING RENAL TRANSPLANTATION. Australian and New Zealand Journal of Surgery. 1984;54(3):223-4.
- Koyle MA, Ward HJ, Twomey PA, Glassock RJ, Rajfer J. Declining incidence of wound infection in cadaveric renal transplant recipient. Urology. 1988;31(2):103-6.
- Midtvedt K, Hartmann A, Midtvedt T, Brekke IB. Routine perioperative antibiotic prophylaxis in renal transplantation. Nephrology Dialysis Transplantation. 1998;13(7):1637-41.
- Novick AC. The value of intraoperative antibiotics in preventing renal transplant wound infections. Journal of Urology. 1981;125(2):151-2.
- Tilney NL, Strom TB, Vineyard GC, Merrill JP. Factors contributing to the declining mortality rate in renal transplantation. New England Journal of Medicine. 1978;299(24):1321-5.
- Landes G, Harris PG, Lemaine V, Perreault I, Sampalis JS, Brutus JP, et al. Prevention of surgical site infection and appropriateness of antibiotic prescribing habits in plastic surgery. Journal of Plastic, Reconstructive and Aesthetic Surgery. 2008;61(11):1347-56.
- Messingham MJ, Arpey CJ. Update on the use of antibiotics in cutaneous surgery. Dermatologic Surgery. 2005;31(8 PART 2):1068-78.
- Perrotti JA, Castor SA, Perez PC, Zins JE. Antibiotic use in aesthetic surgery: A national survey and literature review. Plastic and reconstructive surgery. 2002;109(5):1685-93.
Si tienes comentarios sobre el contenido de las guías de práctica clínica, puedes comunicarte con IETSI-EsSalud enviando un correo: gpcdireccion.ietsi@essalud.gob.pe
SUGERENCIAS
Si has encontrado un error en esta página web o tienes alguna sugerencia para su mejora, puedes comunicarte con EviSalud enviando un correo a evisalud@gmail.com